Systems biology of aging
Course Title: Systems biology of aging and longevity 20263011
Semester: 1st Semester
Credit Points: 2.00
Days,Time,Location: Monday, 1415-1600, Botnar auditorium
Date of first lecture: 27/10/2025

Course Title: Systems biology of aging and longevity 20263011
Semester: 1st Semester
Credit Points: 2.00
Days,Time,Location: Monday, 1415-1600, Botnar auditorium
Date of first lecture: 27/10/2025

Speaker: Prof. Leon Peshkin
Title: Reverse Engineering Anti-Aging Interventions from Pharmaco-biology in Model Organisms
Place: Botnar auditorium
The aging process represents one of biology's most complex system-level phenomena. A major challenge is moving from observing its correlates to identifying its fundamental, targetable bottlenecks. In this talk, I will explore a reverse-engineering approach, using pharmacological interventions in model organisms to deconstruct the mechanisms of aging and pinpoint promising avenues for intervention. I will discuss how we can leverage existing biological data and what new, targeted measurements are required to fill critical gaps. A key question is the selection of appropriate model organisms that offer the right balance of physiological complexity, experimental tractability, and translational relevance for aging research. Furthermore, I will examine the role of artificial intelligence in this endeavor: while AI excels at finding generalizable patterns, its success is critically dependent on the quality and nature of the underlying data—an area where significant improvements are needed. I will present examples from my work across multiple species, including the development of a scalable high-throughput platform for pharmaco-biology in Daphnia. This system allows us to characterize drug-induced perturbations and link them to lifespan and healthspan outcomes. We will discuss a computational framework to regress macro-phenotypes to the molecular pathways. Finally, I will outline central challenges in the field and propose concrete directions for researchers interested in joining the effort to reverse engineer aging.
Leonid Leon Peshkin is a scientist working at the Systems Biology Department at Harvard Medical School.
Peshkin's research interests include embryology, evolution and aging.

Aging is a part of living, and all living organisms do it. But while it’s straightforward to determine the age of an organism - be it the rings on a tree, the lines on a face, or the color of a coat - it is much more challenging to determine and characterize the age of an individual cell, which limits our understanding of the role they play in aging and disease.
Weizmann Institute scientists, led by Dr. Valery Krizhanovsky in the Department of Molecular Cell Biology, developed a means for quantifying and identifying aging cells in tissues on a single-cell basis, with great precision. The method combines measuring amounts of an enzyme whose activity is associated with aging, together with staining for chemical indicators of aging. The method can be used to identify cells in tumor tissue, in fibrous tissue, as well as in healthy tissue. The method paves the way for understanding and controlling the genes that affect the aging process.

Fragile bones, deteriorating posture, and frequent fractures are all well-known hallmarks of old age. In a pair of recent studies, one published in Cell Reports and the other one in Developmental Cell, Prof. Elazar Zelzer and his team in the Department of Molecular Genetics examined the role of a sensory feedback system in muscles that guides both healing fractures and maintains the alignment of the spine.
Each group of long skeletal muscles contains sensory fibers that detect changes in the length of the muscle and report this information to the brain. Called the proprioceptive system, this feedback loop between muscles and the brain plays a key role in guiding the growth and repair of bones, and in maintaining posture. Prof. Zelzer and his group have been studying the repair of fractures for a long time. They noticed that newborn mice had the ability to repair leg fractures naturally. These unstabilized fractures in the humerus were able to undergo spontaneous realignment, which they termed “natural reduction.”
They found that the natural reduction ability was even more marked in three month old mice. They were curious what guided this repair process and discovered that muscle contractions were necessary to help the process along.
The musculoskeletal system contains a large number of proprioceptive mechanosensors. These spindle-shaped sensors are found throughout striated muscles and the Golgi tendon organ (GTO) is a sensor found at tendon junctions. These sensors transmit their feedback to the central nervous system via specialized “proprioceptive” neurons. Prof. Zelzer and his team proposed that the neuronal system and its proprioceptive feedback system act as a super-mechanism orchestrating natural reduction. They were able to use genetic knockouts in mice to show that mutants with the transcription factor Runx3, lacked functional proprioceptors, and therefore failed to realign properly. However, mice with the Egr3 growth factor knocked out lacked muscle spindles but not Golgi tendon organs, and displayed a less severe decrease in their ability to realign bones, suggesting that both receptor types, as well as muscle contraction, are required for this regulatory mechanism.
Taking their research further, they showed that the proprioceptive system plays a key role in maintaining spine alignment. Maintaining posture requires tight regulation of the position and orientation of numerous spinal components. Yet, surprisingly, Prof. Zelzer and his team noted that little is known about this regulatory mechanism. They were able to show that genetically engineered mice that lacked both of the above proprioceptive receptors developed a form of scoliosis.
Their findings clearly indicate that the proprioceptive system may not only provide an array of dynamic spine stabilizers, but also acts as a gatekeeper that prevents progressive spinal deformation.

Detecting the genes for hereditary neurodegeneration is challenging. In the case of ALS (Amyotrophic lateral sclerosis), commonly known as Lou Gehrig's disease, the disease-associated genes that have been identified explain only a small part of the cases. Prof. Eran Hornstein of the Department of Molecular Genetics studies microRNAs, suggesting they influence motor neuron development and survival.
MicroRNAs (abbreviated miRNA) are non-coding RNA molecules that play key roles in the process of gene expression. They are major regulators in a wide spectrum of neuronal processes and are pointed out as involved in diseases such as Alzheimer’s, Parkinson’s, and Huntington’s and also conditions involving motor neurodegeneration.
In a recent research, Prof. Hornstein and his group suggest that an enzyme called Dicer is responsible for the defects linked to miRNAs that are associated with ALS. Prof. Hornstein believes that his findings will yield new candidate ALS genes, providing the basis for additional studies and future therapeutic leads. Moreover, he projects that this research will provide insight into novel pathways for motor neuron degeneration in ALS.
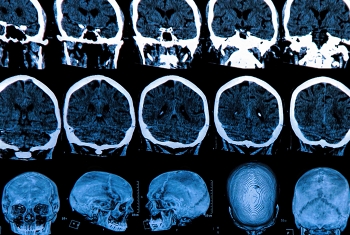
Cognitive decline in Alzheimer’s disease (AD) is associated with a range of physical changes in the brain: a loss of both brain cells and their interconnection points, and the accumulation of tangled neural fibers and plaques of misfolded amyloid-β protein. Most AD therapeutics use immunological and pharmacological tools to target the proteins thought to be responsible for these pathological changes, with mixed results. In addition, treating brain inflammation, which often accompanies neurodegenerative diseases, with nonsteroidal anti-inflammatory drugs has proven ineffective in halting disease progression.
In this review article Prof. Michal Schwartz in the Department of Neurobiology weighs the evidence and suggests revisiting therapeutic options. She recommends shifting focus to the role of the immune system in neurodegenerative diseases such as AD. In particular, she argues that methods for recruiting the brain’s own immune cells, called microglia, to target and destroy tangles and plaques, may be the key to combatting AD.