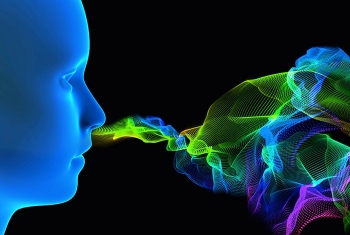
Sniffing out congenital anosmia
A project at the Crown Human Genome Center led by Prof. Doron Lancet of the Weizmann Institute’s Department of Molecular Genetics, in collaboration with clinicians from Meir Hospital in Kfar Saba, has clarified the genetic roots of congenital anosmia—the complete loss of the sense of smell (olfaction) from birth. The scientists revealed a connection between congenital anosmia and Kallmann syndrome, a more-studied condition characterized by olfactory impairment. The researchers found six different genes suspected in both conditions, thus revealing that the genetic basis of congenital anosmia is more complex than previously thought.